Summary
OBJECTIVEThe purpose of the present study was to investigate dosimetric and mechanical stability of CyberKnife Robotic Radiosurgery System (Accuray Inc., Sunnyvale, CA, USA) in short- and longterm period.
METHODS
Output factor measurements and automated quality assurance (AQA) tests performed on CyberKnife
unit 2009-2013 at radiation oncology department of Hacettepe University, Turkey, were
analyzed retrospectively.
RESULTS
According to the analysis, more than 95% of the output measurements over 5 years were within the
tolerance limit ≤2%. In AQA test analysis, 144 AQA test results were within the tolerance limit from
2009 to 2011. However, 7 of the 51 measurements taken in 2012, and 4 of the 47 measurements
performed in 2013 exceeded 1 mm radial error.
CONCLUSION
Output and AQA data of CyberKnife system indicate that it is quite stable in daily and long-term
period. Nevertheless, daily measurements should be performed on CyberKnife unit since high radiation
dose per fraction is usually delivered to target volume.
Introduction
The main purpose of radiotherapy (RT) is to deliver an accurate absorbed dose to the target volume while staying within acceptable tolerance limits for surrounding normal tissue and critical organs in order to minimize collateral effects. Over the last 2 decades, many improvements have occurred in the field of radiation therapy such as new treatment modalities (intensity-modulated radiotherapy [IMRT], volumetric-modulated arc therapy [VMAT] and stereotactic radiosurgery/radiotherapy [SRS/SRT]), new image-guided systems (in-room computed tomography [CT] techniques, magnetic resonance imaging [MRI]-guided RT and ultrasound [US]- based systems), as well as new quality assurance (QA) and quality control (QC) systems. Nevertheless, there are still inevitable uncertainties due to the dosimetric and mechanical stability of the linear accelerator (linac) over a period of time. Therefore, efficient QC programs should be put in place to minimize uncertainty based on machine characteristics and parameters.Dosimetric and mechanical QC of a linac is the process of keeping the accuracy of machine functions within suggested tolerance limits.[1,2] Reports and documents for these suggested values have been published by the International Atomic Energy Agency (IAEA), the American Association of Physicists in Medicine (AAPM), the European Society for Therapeutic Radiology and Oncology (ESTRO), and by several other national and international organizations.[3] The main purpose of all these QA programs is to standardize function of the treatment and measurement equipment used in RT facilities, and thus to maximize quality of patient care. The times tables and tolerance limits of QC for conventional linacs and SRS/ SRT units have been studied widely in the literature. [2,4–10] Moreover, control charts, as used in industrial manufacturing and other healthcare systems, have recently been applied to QA for RT to determine shortand long-term stability of conventional linacs.[11–22] However, there does not appear to be a study analyzing short- and long-term output stability of CyberKnife Robotic Radiosurgery System (Accuray Inc., Sunnyvale, CA, USA).
In SRS/SRT facilities with CyberKnife, high radiation dose is usually delivered to target volume with sub-millimeter accuracy. Therefore, both mechanical accuracy and dosimetric stability of the system play important roles in the precision of the treatment. [4] The present study is an analysis of the short- and long-term output and target positioning stability of CyberKnife unit.
Methods
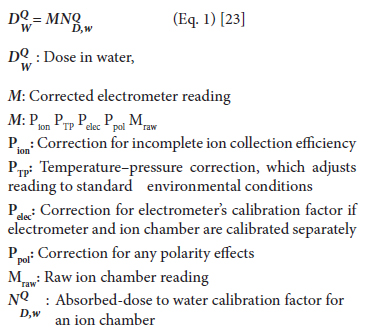
Output stability analysis for CyberKnife Robotic Radiosurgery SystemOutput measurements collected by department of radiation oncology at Hacettepe University, Turkey, between 2009 and 2013 were analyzed to evaluate the short- and long-term output stability of G4 CyberKnife Robotic Radiosurgery unit. Output was calibrated to 100 cGy=100 MU (or 1 cGy=1 MU) at 1.5 cm depth in water using AAPM Task Group (TG) 51 protocol[23] for reference dose calibration as defined in Table 1. In 5 years, measurements were performed on daily basis 976 times using 0.6 cc PTW Farmer ionization chamber (PTW, Freiburg Germany) with buildup cap attached to the birdcage chamber holder, using necessary correction factors according to AAPM TG-51 protocol (Eq. 1).[23] Measurements were repeated 3 times in every daily setup and average value was taken as output value. When the difference between measured output and reference value exceeded threshold of 2%, output calibration was usually performed before starting the treatment. Readings before and after calibration were recorded in output database.
Table 1: Reference conditions for output measurement in Cyberknife unit
Equation for the dose absorbed in water for radiation of quality Q is
AQA test analysis for CyberKnife Robotic
Radiosurgery System
The AQA test is an isocentric targeting accuracy or
robot pointing test to verify delivery accuracy of CyberKnife
unit; it is similar to the Winston-Lutz test[24]
commonly used in gantry-based SRS/SRT systems. In
the present study, 242 AQA tests (from 2009-2013)
performed on CyberKnife system at Hacettepe University
were analyzed retrospectively. Custom designed
AQA phantom containing 2 cm tungsten ball hidden
in cubic phantom was used for the measurements (Figure
1). In the QA, 2 orthogonal gafchromic films were
placed inside the phantom (Figure 1) and an isocentric
treatment consisting of 2 beams in anterior/posterior
and lateral directions were delivered tracking 4 fiducial
markers (Figure 2). Targeting error (Eq. 2) was determined
by analyzing the offset from the center of concentric
circles formed by the shadow of the metal ball and the acrylic target sphere in anterior/posterior, left/
right and superior/inferior directions. If radial error
deviated more than 1 mm from reference value, endto-
end (E2E) tests were performed and the manipulator
was recalibrated. All these data were recorded in
AQA database.

Fig 1: AQA phantom with 2 orthogonal films after exposure.
Fig 2: AQA test geometry in CyberKnife unit.
Results
Output stability analysis for CyberKnife Robotic Radiosurgery SystemDaily output data of the CyberKnife system is shown in Figure 3. In 2 of 976 measurements, differences with respect to reference value of 100 cGy were more than 3%. However, over 5 years, more than 95% of measurements were within tolerance limits (≤2%). Although percentage of measurements exceeding the limit was nearly 5%, dose calibration was performed in only 2% of the measurements. If limits were exceeded due to a change in ambient conditions, such as room temperature and pressure, calibration was not performed until treatment of first patient, and additional measurements were taken prior to every treatment until stabilization of environment conditions. According to analysis of yearly measurements over 5 years (Figure 3), output of CyberKnife system is quite stable in long-term period. In addition to variation of output trend over time as illustrated in Figure 3, statistical analyses of output values on yearly basis were evaluated, and are presented in Table 2.
Fig 3: Daily and long-term output constancy of CyberKnife unit.
Table 2: Statistical analysis of output stability
AQA Test Analysis for CyberKnife Robotic
Radiosurgery System
Between 2009-2011, 144 AQA tests performed on CyberKnife unit were found to be within the tolerance
limit of a radial error of <1 mm. Although 11 of the 98
measurements taken during 2012 and 2013 exceeded
the tolerance limit, 7 of 11 measurements were from
May 2012 and 4 were taken in November 2013. The
manipulator was recalibrated 2 times over 5 years. It
can be seen in Table 3 that there is an increasing trend
in radial error from 2010 to 2013. Nevertheless, yearly
mean radial error variation between consequent years
was less than 0.4 mm and maximum targeting error
was also less than 1.5 mm over the 5-year period. The
present analysis indicates that targeting precision of
CyberKnife system on annual basis was under 1 mm
(Table 3).
Table 3: Yearly basis statistical analysis of targeting error of CyberKnife system
Discussion
In the literature, there are various studies and suggestions based on long-term clinical experience about the process for and frequency of routine QC checks as well as stability analysis of conventional linacs. Although the working principle and safety aspects of CyberKnife system are quite different from other X-ray based accelerators, there is a limited number of studies about QA procedure and stability of CyberKnife unit with respect to the conventional linacs. Therefore, in the present study, we analyzed the short- and long-term output stability and targeting accuracy of CyberKnife robotic radiosurgery system.
The study revealed that output of CyberKnife unit
was quite stable based on daily and annual measurements
(Figure
In addition to output stability, SRS/SRT facilities
with CyberKnife require high degree of targeting accuracy
or mechanical stability with respect to conventional
linac-based treatment techniques such as 3-dimensional
conformal radiotherapy (3DCRT), IMRT,
and VMAT. As small positioning errors in SRS/SRT
equipment can result in considerable changes to calculated
dose of target volume and affect adjacent critical
organs due to steep dose gradient and small target
volume. For this reason, effective QC program should
be implemented to ensure that the accuracy of the CyberKnife
system does not deviate significantly from
the baseline. AQA test is useful to check the spatial
coordinate system of the manipulator. In addition, detailed
analysis of AQA test results can provide valuable
information about the short-term and long-term mechanical
stability of the CyberKnife unit. In the present
study, mechanical stability of CyberKnife system
on yearly basis was analyzed and results indicated that
pointing accuracy of Cyberknife system was well below
the tolerance limit of 1 mm, as recommended by
AAPM TG-135, between the years of 2009 and 2011.
However, 11 of the 98 measurements taken in 2012 and
2013 exceeded tolerance value; 7 were taken in May
2012 and remaining 4 were taken in November 2013.
The manipulator, hence, was recalibrated only twice
over 5 years. Although, AQA test provide valuable information
about targeting accuracy, several parameters
should be controlled before each calibration and E2E
tests should be performed to ensure whether this deviation
is caused by the robot or other factors like film
scanner, film displacement and kilovoltage (kV) imaging
system.
Overall, analysis showed that output and mechanical
stability of CyberKnife was very reliable over 5 years.
Nevertheless, daily output measurements and AQA
test are strongly recommended by the AAPM TG-135.
AQA test is a quick test to evaluate the pointing accuracy
of CyberKnife unit. However it has several limitations
or disadvantages. The first is that it only provides
information on translational parameters (left-right,
superior-inferior and anterior-posterior) of the robotic
system. Second, it is very costly and time-consuming
to take daily measurements. Based on these limitations,
AQA tests should be modified by the manufacturer to
verify both translational and rotational parameters and
a new simple module designed for a quick check of
both mechanical and output stability of the system.
Conclusion
Output data of CyberKnife system is quite stable in daily measurements and in the long-term. In spite of its stability, daily measurements should be performed in SRS/SRT units like CyberKnife Robotic Radiosurgery System since high radiation dose of about 5-34 Gy/fr is usually delivered to target volume. It can be also pointed out that although 11 of 242 AQA tests exceeded the tolerance limit, long-term mechanical stability of the system is reliable, since maximum radial error was below 1.5 mm over 5 years.
Acknowledgements
This study was supported by Hacettepe University Scientific
Research and Development Office Grant Project:
1-05 A 101 009.
Conflict of interest: None declared.
References
1) Sanghangthum T, Suriyapee S, Srisatit S, Pawlicki T.
Retrospective analysis of linear accelerator output
constancy checks using process control techniques. J
Appl Clin Med Phys 2013;14(1):4032.
2) Kapanen M, Bly R, Sipilä P, Järvinen H, Tenhunen M.
How can a cost/benefit ratio be optimized for an output
measurement program of external photon radiotherapy
beams? Phys Med Biol 2011;56(7):2119–30.
3) Huq MS, Fraass BA, Dunscombe PB, Gibbons JP Jr,
Ibbott GS, Medin PM, et al. A method for evaluating
quality assurance needs in radiation therapy. Int J Radiat
Oncol Biol Phys 2008;71(1 Suppl):170–3.
4) Kapanen M, Tenhunen M, Hämäläinen T, Sipilä P,
Parkkinen R, Järvinen H. Analysis of quality control
data of eight modern radiotherapy linear accelerators:
the short- and long-term behaviours of the outputs
and the reproducibility of quality control measurements.
Phys Med Biol 2006;51(14):3581–92.
5) Institution of Physics and Engineering in Medicine
and Biology (IPEMB). Physical aspects of quality control
in radiotherapy. IPEMB Report 81. New York:
1999.
6) Kutcher GJ, Coia L, Gillin M, Hanson WF, Leibel S,
Morton RJ, et al. Comprehensive QA for radiation oncology:
report of AAPM Radiation Therapy Committee
Task Group 40. Med Phys 1994;21(4):581–618.
7) Netherlands Commission on Radiation Dosimetry
(NCS). Quality control of medical linear accelerators:
current practice and minimum requirements. NCS
Report 9. Delft 1996.
8) Swiss Society of Radiobiology and Medical Physics
(SSRMP/SGSMP). Quality control of medical electron
accelerators. SSRMP Recommendations No.11. Bern
2003.
9) World Health Organisation (WHO). Quality Assurance
in Radiotherapy. Geneva 1988.
10) Biggs PJ. Review of the energy check of an electron-only
linear accelerator over a 6 year period: sensitivity of the
technique to energy shift. Med Phys 2003;30(4):635–9.
11) Pawlicki T, Whitaker M, Boyer AL. Statistical process
control for radiotherapy quality assurance. Med Phys
2005;32(9):2777–86.
12) Benneyan JC, Lloyd RC, Plsek PE. Statistical process
control as a tool for research and healthcare improvement.
Qual Saf Health Care 2003;12(6):458–64.
13) Noyez L. Control charts, Cusum techniques and funnel
plots. A review of methods for monitoring performance
in healthcare. Interact Cardiovasc Thorac Surg 2009;9(3):494–9.
14) Tennant R, Mohammed MA, Coleman JJ, Martin U.
Monitoring patients using control charts: a systematic
review. Int J Qual Health Care 2007;19(4):187–94.
15) Boggs PB, Wheeler D, Washburne WF, Hayati F. Peak
expiratory flow rate control chart in asthma care: chart
construction and use in asthma care. Ann Allergy
Asthma Immunol 1998;81(6):552–62.
16) Holli K, Laippala P, Ojala A, Pitkänen M. Quality
control in health care: an experiment in radiotherapy
planning for breast cancer patients after mastectomy.
Int J Radiat Oncol Biol Phys 1999;44(4):827–33.
17) Pawlicki T, Whitaker M. Variation and control of process
behavior. Int J Radiat Oncol Biol Phys 2008;71(1
Suppl):210–4.
18) Breen SL, Moseley DJ, Zhang B, Sharpe MB. Statistical
process control for IMRT dosimetric verification. Med
Phys 2008;35(10):4417–25.
19) Pawlicki T, Yoo S, Court LE, McMillan SK, Rice RK,
Russell JD, et al. Moving from IMRT QA measurements
toward independent computer calculations using
control charts. Radiother Oncol 2008;89(3):330–7.
20) Gérard K, Grandhaye JP, Marchesi V, Kafrouni H,
Husson F, Aletti P. A comprehensive analysis of the
IMRT dose delivery process using statistical process
control (SPC). Med Phys 2009;36(4):1275–85.
21) Able CM, Hampton CJ, Baydush AH, Munley MT. Initial
investigation using statistical process control for
quality control of accelerator beam steering. Radiat
Oncol 2011;6:180.
22) Nordström F, af Wetterstedt S, Johnsson S, Ceberg C,
Bäck SJ. Control chart analysis of data from a multicenter
monitor unit verification study. Radiother Oncol
2012;102(3):364–70.
23) Almond PR, Biggs PJ, Coursey BM, Hanson WF, Huq
MS, Nath R, et al. AAPM’s TG-51 protocol for clinical
reference dosimetry of high-energy photon and electron
beams. Med Phys 1999;26(9):1847–70.
24) Dieterich S, Cavedon C, Chuang CF, Cohen AB,
Garrett JA, Lee CL, et al. Report of AAPM TG 135:
quality assurance for robotic radiosurgery. Med Phys
2011;38(6):2914–36.





